Joint pain and fatigue:
Relieve symptoms with the right diet…
Perhaps you know this?
You feel tired and dull all the time and just drag yourself through the day. Your body feels heavy and immobile, and you often feel tired and stiff when you wake up in the morning. Your body’s ability to recover is significantly reduced. In addition, there are those joint pains that keep coming back, accompanied by swelling and muscle tightness. Your limbs also ache and you may even experience a kind of “whole body pain”.
You suffer from exhaustion and joint pain! And even worse: The complaints have become a permanent condition. Now you ask yourself the question: What can I do myself to alleviate my symptoms? And this is where nutrition comes into play, which can make a decisive contribution…

Joint pain as a constant companion: An enormous burden
Fatigue and its causes
Where or how does our power actually originate?
If you were to ask many different people this question, then you would certainly get the most diverse answers to it depending on, for example, creed or conviction, origin or profession. For the indigenous population, power bears the name Pachamama (Divine Mother), in Chinese medicine one speaks of “Chi”, some people think of power as a muscle-building workout in the gym or of “recharging one’s batteries” in the sun, and still others find their power in prayer or in nature. In the physical sense and according to Isaac Newton, force means: “The temporal change of an impulse”.
If we ask ourselves this question from a scientific-biological perspective, we quickly end up with the mitochondria.

If the exhaustion remains, then mitochondria are often limited in their functioning.
Excursus Mitochondria:
Mitochondria are cell organelles, the so-called “power plants of the cell” or also called “source of female energy”. Each cell of the human body houses an average of about 1500 mitochondria. In these mitochondria, energy in the form of the molecule adenosine triphosphate (ATP) is continuously produced every second in a highly complex chemical process. The supply of all our organs therefore depends on them.
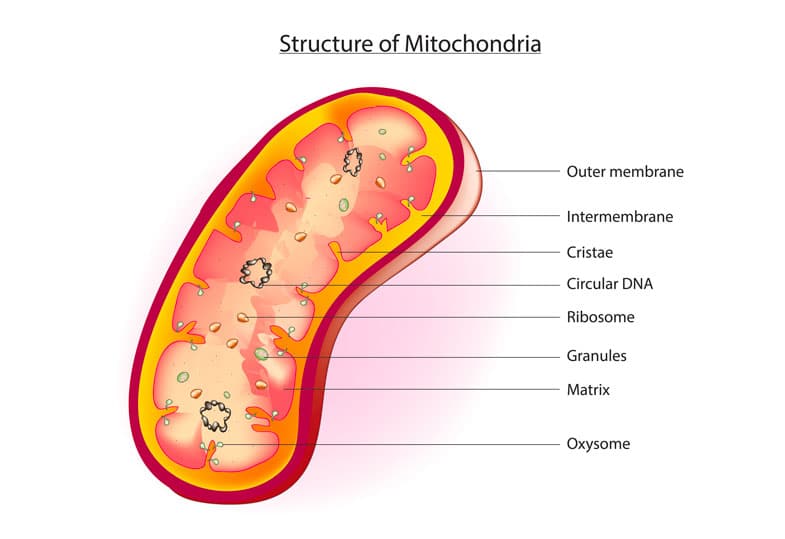
However, today our power plants are very stressed and in the case of many chronic diseases the energy supply in the mitochondria is disturbed.
External stresses and environmental toxins have increased to a great extent: Heavy metals, solvents, electrosmog or water pollution do not remain without effect. But also chronic infections, emotional stress as well as a physical trauma in the area of the cervical spine as well as the decreasing nutrient density of our food (micronutrient deficiencies) can cause a dysfunction.
From a biochemical point of view, due to the progressive dysfunction of the mitochondria, the oxidative and nitrosative stress increases more and more and this directly affects the cellular metabolism. And even more, mitochondria also contain genetic material that is relatively free and unprotected in the matrix and can be damaged by all the stressors mentioned. This existing genome enables the mitochondria to decide whether a cell lives or dies. Now imagine the immense impact such damage caused has on the fate of the cells and thus on our health.
What are the consequences? Impaired hemoglobin formation, decreased synthesis of hormones, worsened breakdown of cholesterol, and much more. And this, in turn, means exhaustion and diseases develop.

Joint pain may be related to a systemic, inflammatory event such as autoimmune disease.
And why do I also have joint pain?
The combined symptoms of “exhaustion and joint pain” (often accompanied by joint stiffness, muscle or whole-body pain) are frequently seen in daily practice when chronic inflammation underlies the mitochondrial disorder. Autoimmune processes (such as in rheumatoid arthritis), chronic infections with pathogens such as Borrelia, Chlamydia, Mycoplasma, EBV or the SARS-CoV-2 virus, or a high load of environmental toxins on the body trigger significant inflammatory processes throughout the body. In this process, joints and muscles can also be directly affected and “attacked”, because in fact the blood vessels in the joints are extremely thin-walled. The wall of these finest arterioles consists of only a single cell layer, which is very permeable to toxins or antigens, so that they can very easily enter the joint space. If the joint pain is due to an autoimmune reaction, the body’s own immune system produces antibodies that are directed, for example, against proteins in the joint and trigger local inflammatory processes.
Sometimes there is also an (additional) hypersensitivity to perceptual stimuli, as in the complaint of fibromyalgia.
The common factor is that we always speak of an increased inflammatory reaction and immune activity. Accordingly, the reduction of this inflammation in the body plays a major role with regard to the improvement of symptoms. And here, nutrition is a very important component.
In addition, the complaints are often also aggravated by an increased acid load and an over-acidified organism, for example through excessive consumption of animal foods.
People who suffer from rheumatic pain,
are in principle always chronically overacidified.
The excess acid is deposited in the tissues and joints, and as a result the muscles become more and more cramped. And people who have already had an attack of gout are familiar with the following phenomenon: the uric acid precipitates and forms “urate crystals” in the joints. A painful inflammatory reaction is the result.

Too much acid can lead to arthritis or osteoarthritis, because it is not uncommon for excess acids to be deposited in the connective tissue and joints in the form of so-called slags.
What does the gut have to do with joint pain?
Also the intestinal health does not remain unmentioned in the context of the “correct nutrition with joint pain and tiredness”.
Most people know it, the famous tiredness after eating. If we eat too much, too fast or something “wrong”, we don’t feel invigorated afterwards, but rather sluggish and stuffed. Then it takes a coffee or two or a nap to return to normal performance.
What is the reason?
For various reasons, our digestive function is limited (unhealthy food, antibiotics intake, eating without feeling hungry or too much, and much more). Thus, the food can not be digested as it should be and so it is an additional burden on the organism. Sometimes there may be parasites in our body, which additionally “eat away” the nutrients and disturb our intestinal environment. If our intestines are not in order, the performance of our immune system is also always reduced and so viruses and bacteria can settle or spread more easily and weaken our body again additionally.
In this context, it is important to mention the topic of “food allergies”. Gluten is a good example of this. The proportion of gluten in food has increased more and more in recent decades. However, the component gliadin in gluten can trigger severe inflammations in the intestine. In addition, antibodies (IgG) against gluten are often detectable. If such food-antibody complexes are then found in the blood, they like to be deposited somewhere and not infrequently in the joints. Joint pain (“of unknown cause” ) is the result. This means that certain foods can trigger both a gradual inflammatory process in the body and an inflammatory episode or pain attack. For this reason, patients with joint pain are often recommended an elimination diet. If a condition repeatedly worsens after eating certain foods, then these should be consistently avoided. At the THERA Praxisklinik in Berlin, we specifically look for food intolerances in our patients. By means of a blood test, we determine which foods the body reacts to with an inflammatory reaction.

The consumption of certain foods can trigger inflammation in the body. This activates the immune system and fatigue can be the result.
What is the right diet for joint pain and fatigue?
No matter what complaints or diseases are present in your case: Of course, it always requires an individual nutritional consultation and assessment of the overall situation with consideration of underlying and concomitant diseases. Ultimately, joint pain can conceal a wide variety of medical conditions, and fatigue can be an expression of a wide range of organ dysfunctions. Nevertheless, the right diet is always an important building block towards a better quality of life and symptom relief. Certain recommendations therefore have a certain general validity. You will find a few helpful tips in the following overview.

The different fats in our diet can be either pro- or anti-inflammatory in the body.
Diet tips: What to do for joint pain
Regulate inflammation via fatty acid composition:
Fats are essential for health. And yet, not all fats are the same. Here it is important to look carefully and use the “good” fats. After all, fats can fuel inflammatory processes in the body or, in the better case, contain and regulate them.
- Saturated fats can trigger a danger signal in our immune cells and cause an inflammatory reaction. And trans fats (= hydrogenated vegetable oils) have also been shown to have negative consequences for our immune response. So when we consume these two types of fats in high levels, we provoke inflammation in the body.
- Also problematic is the high consumption of omega-6 fatty acids. You could call them the raw material for inflammatory reactions, because they contain linoleic acid, which is metabolized to arachidonic acid and corresponds to a signal molecule that promotes inflammation. We absorb arachidonic acid with our food when we consume animal fats or certain vegetable oils such as sunflower oil or even margarine. So by reducing or eliminating these foods, arachidonic acid can be slowed down. This is one of the reasons why many patients are recommended a vegetarian, vegan or Mediterranean diet.
- At the same time, there is an antagonist of these pro-inflammatory signal molecules: omega-3 fatty acids. These should therefore be consumed in abundance! Our immune system uses omega-3 fatty acids to produce special anti-inflammatory mediators. They are mainly found in fatty cold-water fish such as salmon or herring. Unfortunately, bioavailability from plants is much lower. Nevertheless, a certain part can be covered from vegetables, nuts and seeds such as linseed or walnut oil.
In studies of rheumatism patients, fish oil significantly reduced morning joint stiffness, joint redness and swelling, and pain.
Ultimately, however, what matters most is the ratio of omega-3 to omega-6. Both fatty acids are important for our health. However, our diet today actually contains less omega-3 and much more omega-6, so blood tests of fatty acid status usually show a significantly shifted ratio in favor of omega-6 fatty acids.
Regulate acid-base balance:
If we eat a lot of acid-forming foods, then this can set additional inflammatory stimuli and weaken bones, cartilage and connective tissue. An alkaline diet is therefore preferable. Bad acid-forming foods are, for example, alcohol, sugar, coffee, carbonated drinks or dairy, eggs and meat from conventional farming. These should be avoided as far as possible or consumed only in small quantities.
Prevent insufficiency:
As a result of chronic inflammatory processes, long-term medication or even psychological stress and loss of appetite, there may be an undersupply of energy or nutrients. By means of BIA measurement (bioelectrical impedance analysis), the body composition can be specifically examined. Among other things, this simple examination method provides information on how much fat, water and active cell mass is present. From this, conclusions can be drawn about the nutritional status of the cells or, for example, a possible protein deficiency.
Anti-inflammatory foods for the diet:
- Turmeric, ginger, cinnamon
- Citrus fruits like lemons, oranges or grapefruit
- Onions and garlic
- All cabbage and green leafy vegetables like spinach
- Cherries, papaya, various berries
- Legumes and fermented foods
- U.v.a.m.
Support intestinal microbiome:
In most patients with chronic complaints/pain, the intestinal environment is also disturbed and thus the microbiome is not healthy. Here the secret weapon is dietary fiber. They regulate the composition of the intestinal bacteria and stimulate digestion. The breakdown of dietary fiber by bacteria also produces short-chain fatty acids. These have an anti-inflammatory effect, serve as a source of energy for the intestinal cells and regulate the intestinal barrier. So there is no way around a diet rich in dietary fiber! (By the way, fiber also supports weight reduction, lowers the risk of colon cancer and cardiovascular diseases, binds harmful substances and toxins, and lowers cholesterol levels).
A very good source or supplement for the intake of dietary fiber are, among others, bran, flaxseed or psyllium husks. It is always important to ensure sufficient fluid intake.
Therapeutic fasting:
A fasting cure or also intermittent fasting can contribute decisively to relieve the symptoms and also to lower the inflammation parameters in the blood.

Are you looking for a doctor in Berlin who cares for you holistically?
We support you in the THERA Praxisklinik in Berlin.
As you can see from the above examples, it takes a very comprehensive and holistic view to really get to the bottom of the cause of joint pain and fatigue. At the THERA Praxisklinik, we have extensive experience with patients suffering from precisely these symptoms (and not infrequently diffuse complaints associated with them) and our doctors take a lot of time to really consider all aspects and to track down even the smallest disturbing factors and fields.
Following a detailed medical history interview and a physical examination, your attending physician will perform comprehensive laboratory and intestinal diagnostics to gather further information: What is the condition of the mitochondria and how does energy production take place? How high is the free radical load? Are there micronutrient deficiencies? What is the hormone status? How high is the load of heavy metals? Are there chronic inflammations? Are autoimmune processes present? Is the body burdened by pathogenic agents? How healthy or diseased is the gut microbiome? What is the nutritional status?
At all levels, we take a thorough look at the influencing factors and then create a suitable therapy plan. In addition, we always want to strengthen the mitochondria in their function and provide them with the substances (“fuels”) they need for function and regeneration: Micronutrients and oxygen!
We discuss with each of our patients the optimization of their nutritional habits, especially with regard to intestinal health, which is significantly involved in inflammatory processes in the body. Individual and targeted nutritional counseling can be provided by our nutritionist.
We increase the oxygen content in the cells by carrying out equipment-supported “altitude training” with our patients. For this purpose, the MITOVIT hypoxia training (Interavall Hypooxia/Hyperoxia Therapy IHHT) is used in the rooms of the THERA Praxisklinik in Berlin.
For the treatment of pathogenic agents, we have at our disposal, in addition to a wide variety of herbal or homeopathic medicines, ozone autologous blood therapy.
Medical ozone has a strong bactericidal, fungicidal and virus-inactivating effect. In addition, small amounts of ozone, administered as a self-blood treatment, activate the body’s own antioxidants and radical scavengers.
Weiterführende Themen (Auswahl):
Your contact persons
Contact and appointment possible at any time
Do one or more of the above points apply to you and would you like to do something for your health? Are you curious? Please feel free to contact us by phone to make an appointment.
You can reach us according to our opening hours at tel. 030 79016533. We look forward to your call or message.
References:
Dietary Short-Term Fiber Interventions in Arthritis Patients Increase Systemic SCFA Levels and Regulate Inflammation. Dürholz K. et al. Nutrients 2020 Oct 20;12(10):3207. doi: 10.3390/nu12103207.